are you in favor of giving contraceptive to teenagers?
Saturday, March 21, 2009
HIV treatment during pregnancy
Saturday, March 14, 2009
worst than cancer
What is HIV?
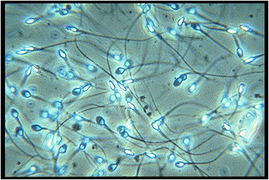
The Human Immunodeficiency Virus (HIV) is the virus that leads to AIDS. HIV belongs to a subset of retroviruses called lentiviruses (or slow viruses), which means that there is an interval -- sometimes years -- between the initial infection and the onset of symptoms. Upon entering the bloodstream -- through mucous membranes or blood-to-blood contact -- HIV infects the CD4+T cells and begins to replicate rapidly.
Scientists believe that when the virus enters the body, HIV begins to disable the body's immune system by using the body's aggressive immune responses to the virus to infect, replicate and kill immune system cells. Gradual deterioration of immune function and eventual destruction of lymphoid and immunologic organs is central to triggering the immunosuppression that leads to AIDS.
What is AIDS?
Acquired Immunodeficiency Syndrome (AIDS) is the final stage of HIV infection. The Centers for Disease Control establish the definition of AIDS, which occurs in HIV-infected persons with fewer than 200 CD4+T cells and/or persons with HIV who develop certain opportunistic infections. In 1992, the CDC redefined AIDS to include 26 CDC-defined AIDS indicator illnesses and clinical conditions that affect persons with advanced HIV.
What is a retrovirus?
A retrovirus is any of a group of viruses that contain two single-strand linear RNA molecules per virion, which means it carries its genetic blueprint in the form of ribonucleic acid (RNA) instead of deoxyribonucleic acid (DNA). Additionally, the enzyme reverse transcriptase is employed to copy its genome into the DNA of the host cell's chromosomes. Usually the cellular process involves transcription of DNA into RNA. Reverse transcriptase makes it possible for genetic material to become permanently incorporated into the DNA genome of an infected cell.
What is the distinction between HIV and AIDS?
AIDS is a disease developed by a person living with HIV, which is a viral organism. The term AIDS applies to the most advanced stages of HIV infection. Although an HIV-positive test result does not mean that a person has AIDS, most people will develop AIDS as a result of their HIV infection.
There are four main stages in the progression of an HIV infected person developing AIDS. The period following the initial HIV infection is called the window period. It is called this because this period reflects the window of time between infection with the virus and when HIV antibodies develop in the bloodstream. An HIV test that looks for antibodies taken during this time can result in a false negative, though antibodies usually appear within six months of the initial infection.
Seroconversion refers to the period of time during which your body is busy producing HIV antibodies, trying to protect itself against the virus. This is the period after the initial infection when many people experience flu-like symptoms and swollen lymph nodes – this is a highly infectious stage.
After most people seroconvert, they usually experience a symptom-free period or asymptomatic period. This stage can last anywhere from 6 months to over 10 years, varying from person to person. Although the person with HIV is experiencing no symptoms, the virus is still replicating inside the body and weakening the immune system.
After this period, severe CD4+T cell loss leads to the symptomatic period, in which the body experiences the symptoms associated with HIV. This is the final stage before developing AIDS.
How is HIV transmitted?
HIV infection most commonly occurs through sexual contact. However, the virus can also be spread through blood-to-blood contact -- such as sharing needles or blood transfusions involving unscreened blood. Studies have shown that HIV is not transmitted through casual contact such as touching or sharing towels, bedding, utensils, telephones, swimming pools, or toilet seats. Scientists have also found no evidence of transmission through kissing, sweat, tears, urine or feces. It is important to acknowledge that it is not sex that transmits HIV, but certain bodily fluids: blood, semen (including "pre-cum"), vaginal secretions and breast milk. High-risk behaviors that can result in HIV transmission are sharing needles for drugs, tattoos, body piercing, vitamins or steroids with an HIV-infected person and/or engaging in unprotected anal, vaginal or oral sex with a person who is HIV infected. The virus also can be transmitted from an HIV-infected mother to her child through pregnancy, birth or breastfeeding.
It does appear that persons already infected with a sexually transmitted disease are more susceptible to acquiring HIV during sex with an infected partner. Mucous membranes, a weak point in the skin, include the lips, mouth, vagina, vulva, penis or rectum. Because mucous membranes are porous and viruses and other pathogens are able to pass through, these areas are rich in immune cells. When a person already has a sexually transmitted disease, sex organs may be flooded with CD4+T cells, making it much easier for HIV to infect.
The only way to determine HIV infection is to be tested for the virus. It is not unusual for HIV-infected persons to experience symptoms years after the initial infection; some may be symptom free for over 10 years. However, during the asymptomatic period, the virus is actively multiplying and destroying cells in the immune system, weakening the body's ability to fight infection. The effect is most keenly observed in the decline of the immune system's key infection fighters in the blood, the CD4+T cells. There are medical treatments that can reduce the rate at which HIV disables the immune system; early detection offers more options for treatment and preventative care. As a matter of safety, people who engage in high-risk behaviors -- such as intravenous drug use or having unprotected sex with multiple partners -- should be tested regularly.
How can I lower my risk of HIV infection?
Practicing safe sex and avoiding high-risk behaviors are the keys to protecting yourself from HIV. This begins with understanding that there is a risk of transmission any time infected blood, semen, vaginal secretions or breast milk are exchanged. By limiting the possibility of these fluids entering your bloodstream, you are lowering the possibility of HIV infection. You can achieve this by limiting the number of people you have sex with, never sharing needles with anyone at any time and avoiding the use of alcohol or drugs before having sex. Drugs and alcohol may influence your decision and may reduce your ability to practice safer sex.
Safe sex involves using a latex condom or latex square (dental dam) for sexual activities -- when used properly, latex is an effective barrier against the spread of HIV. In addition, the use of lubricants should be limited to water-based only, as oil-based lubricants can break down latex condoms within seconds of use.
What are the symptoms of HIV?
The only way to determine HIV infection is to be tested, as symptoms and latent periods vary from person to person. It is common during the first two to four weeks of infection that people experience flu-like symptoms and enlarged lymph nodes. This is because the virus migrates to various organs in the body, particularly the lymphoid organs. During this stage people are highly infectious and HIV is present in large quantities in genital secretions.
According to the Centers for Disease Control and Prevention, the following are symptoms that may be warning signs of HIV infections:
· Rapid weight loss
· Dry cough
· Recurring fever or profuse night sweats
· Profound and unexplained fatigue
· Swollen lymph glands in the armpits, groin or neck
· Diarrhea that lasts for more than a week
· White spots or unusual blemishes on the tongue, in the mouth or in the throat
· Pneumonia
· Red, brown, pink or purplish blotches on or under the skin or inside the mouth, nose or eyelids
· Memory loss, depression and other neurological disorders
Remember that the only way to determine HIV infection is to be tested for the virus. No one should assume they are HIV positive or negative based on the presence or absence of any of the above symptoms. Each symptom can be related to other illnesses; similarly, other symptoms or the absence of symptoms cannot assure that someone is HIV negative. To be certain, get tested.
I just found out I am HIV positive -- what should I do?
The most effective weapon you have against HIV is knowledge -- understanding how the virus progresses and operates, learning how to monitor your health and staying informed of your treatment options. An important step is finding a doctor that specializes in HIV treatment. There are a number of resources available to you; you can ask your family doctor, request information from a government agency (such as your local department of health), or contact a regional or national HIV/AIDS service organization.
Your doctor can be a good source of information, but you should be proactive in staying up to date on drug therapies and treatment options. Don't be afraid to ask questions and discuss treatment strategies with your physician-- this is an important step in taking charge of your own health.
Equally as important is emotional support -- from friends, family or a group. There are a number of HIV/AIDS support groups, both locally and nationally, which can offer assistance in dealing with the many new aspects of life after you have tested positive. An opportunity to interact with people who are going through or have been through a similar experience is invaluable.
Many people continue to live healthy, happy lives more than 10 years after testing positive for HIV. The bottom line is that testing positive for HIV is not a death sentence. Treating your body well, following your doctor's instructions and maintaining good mental health are simple steps you can take to manage your health. Different things work for different people -- find out what works for you and do it.
Saturday, March 7, 2009
HIV
chickenpox and pregnancy
Is there a concern with chickenpox and pregnancy? If I develop chickenpox while I'm pregnant, could it harm the baby?
Answer
from Roger W. Harms, M.D.
Chickenpox (varicella) is a highly contagious viral illness that causes an itchy rash. Most pregnant women are immune to chickenpox, due to either immunization or a childhood bout with chickenpox. If chickenpox develops during pregnancy, the risks depend on the timing.
If chickenpox develops during the first 20 weeks of pregnancy, the baby faces a slight risk of congenital varicella syndrome — a rare group of serious birth defects. A baby who has congenital varicella syndrome may experience:
- Scars on the skin
- Muscle and bone defects
- Malformed limbs
- Vision problems
- Mental retardation
If chickenpox develops shortly before delivery, the baby may be born with a potentially life-threatening infection.
If you're considering pregnancy and you're not immune to chickenpox, ask your doctor about the chickenpox vaccine. It's safe for adults, although you'll need to wait at least one month after vaccination before trying to conceive. If you're unsure of your immunity, your doctor can do a simple blood test to find out.
If you're exposed to chickenpox during pregnancy and you're not immune to the illness, contact your doctor immediately. He or she may recommend an injection of an immune globulin product that contains antibodies to the chickenpox virus. When given within 96 hours after exposure, the immune globulin can prevent chickenpox or reduce its severity.
If you develop chickenpox during pregnancy, your doctor may prescribe oral antiviral drugs to reduce the severity of the illness. This may help reduce the risk of complications, such as pneumonia.
If your baby is born with chickenpox, he or she may be treated with an immune globulin. When given promptly, the immune globulin usually reduces the severity of the illness. If needed, antiviral drugs may be given as well.